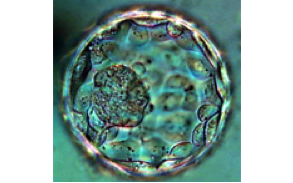
Blastocyst Culture
What is Blastocyst culture and transfer?
Traditionally, embryos had been transferred to the uterus on the second or third day of development after egg retrieval and the embryos that were not transferred they would be frozen for future use. BL culture and transfer consists of keeping the embryos for two or three additional days in culture (Day 5 or Day 6) to allow them to reach the blastocyst stage.
Is this a new technique?
It can hardly be considered as a new technique since we have been using it since 1992 or earlier by others.

What is the clinical value of Blastocyst culture?
Blastocyst culture and transfer is an important technique which main value is in minimizing the risk of multiple pregnancy. The ability to grow embryos for five or six days to the blastocyst stage of development in the laboratory, rather than the traditional three days, allows FERTILITE's embryology team to determine, with greater certainty, which embryos are really the "best" in terms of their potential for implantation. Consequently, blastocyst culture makes it possible to select the best one or two blastocysts vs. two or three (or rarely four) early embryos to transfer back to the mother. This reduces the occurrence of potentially risky multiple births.
Are there any other advantages of Blastocyst Culture and Transfer?
Yes, as the embryos spend more time in culture they have a better chance of displaying their growth potential. We used to believe that the reason for embryos non-developing normally in culture was due to poorly designed culture media or any other unknown environmental factors associated with our culture systems. Research has shown that the reason embryos do not continue to grow in vitro is mainly due to genetic or chromosomal abnormalities and not our media or culture conditions. So, by performing embryo transfers on Day 2 or 3 we were transferring embryos that could not be fit for transfer and in order to mitigate that problem more than 2-3 would be selected for transfer. This practice would end up in some cases in high order risky pregnancies with 3 or more fetuses. Moreover, as embryo freezing was done on day 3 we would end up freezing many unfit embryos that would give the patient an unrealistic sense of security by having “a lot of embryos frozen” non realizing that many of them would not survive a pregnancy.
Three important factors had limited the number of embryos that will survive to this stage:
First, the inherent "health" of any embryo will dictate its ability to continue to grow and divide. It is estimated that nearly 35% of the embryos are destined to stop growing in patients 30 years old or
younger. As the patient age increases the proportion of embryos destined to stop cleaving increases. The reason for this is mainly defective chromosome numbers (See Aneuploidy) Several eggs may have initially fertilized, but only a few will progress to the four-cell stage on day two in culture, fewer still to the eight-cell stage on day three in culture, and even fewer will develop into blastocysts. Simply put, this self-selection can be viewed as "survival of the fittest".
The second limiting factor in preventing continued growth of embryos in culture had been the culture media itself. Researchers have identified shortcomings of the in vitro culture environment we have developed new culture solutions called Blastocyst Media. These are rich in life sustaining nutrients that give the embryos every chance to reach their full inherent potential. From egg collection onward, the embryo will now be exposed to specific media that are designed to meet the nutritional requirements of each stage of development.
Third, even with embryos of good growth potential and optimal culture media, the experience and expertise of the laboratory embryologists doing this important work is critical to achieving good blastocyst development. It is here that the embryologists at FERTILITE excel. They, as opposed to many other laboratories who have tried but then abandoned the rigors of blastocyst culture, have optimized the opportunities for patient success in their IVF cycles and in their quest to build their families.
What Are the Benefits of Blastocyst Transfer?
Let's use an example. A patient who has 15 eggs retrieved, an average of 12 will fertilize. It is impossible to determine at this point which of these 12 are most likely to implant and develop into a baby. Perhaps all will, but most likely they will not. On the traditional day of embryo transfer (day three), 8 out of the twelve initially fertilized may be developing into embryos with 7-, 8- or 9-cells. The others may have slowed or stopped their development altogether as naturally many eggs and embryos are abnormal.
In this example, on day three (day of the typical embryo transfers) we are left with several embryos that still look like they may have excellent potential. Which ones to transfer? Which ones are really the "best"? It is difficult to ascertain which ones will continue their development. Two additional days in the blastocyst culture medium allows the natural selection process to continue. Thus, after 5 or 6 days of growth in the laboratory, only 4-5 of the original ten embryos may remain viable, showing their inherent potential. We now know the best embryo(s) to transfer.
Embryos transferred at the blastocyst stage have made it through key developmental stages of development and typically offer a greater chance of implanting. Therefore, we need only return 1 or 2 blastocysts to the mother instead of the typical 2 or 3 early embryos without affecting pregnancy rates. In addition, the fewer embryos transferred the more may available for cryopreservation for future use.
As pregnancy rates of Day 3 vs Day 5 transfers are similar, the most significant benefit of blastocyst culture and transfer is the reduction of multiple births that can result from in vitro fertilization. This means that the many obstetrical complications that may arise from multiple pregnancies can be minimized. It is especially important in helping patients avoid having to make the difficult personal and ethical decisions regarding selective reduction.
Is Blastocyst Culture and Transfer for Everyone?
Definitely YES! In thinking of the example above, patients who have fewer oocytes retrieved, fewer fertilized or fewer dividing embryos by day three are better off to leave the embryos TWO more days in culture and know that there are (or not) embryos at the blastocyst stage for transfer rather than transferring any embryos on day 3 and prolong the agony for 10-12 additional days of stress and medical expenses.
The new culture systems do NOT improve the health or viability of an individual embryo but it DOES NOT affect the ability of a good embryo to reach the blastocyst stage.
It is a nice option to be able to do blastocyst transfer since that means that there were a larger number of eggs retrieved, a larger number fertilized and growing on day 2 and 3 of culture that we want to follow. However, a large proportion of patients with fewer eggs and/or fewer embryos are better served by allowing their embryos to be cultured for 2-3 additional days. All of the embryo transfers at FERTILITE are done on days 5 or day 6. (The day 6 blastocyst transfer is recommend when, on day 5, the embryos still may not have revealed which are the best of the group for transfer, and one more day is recommended).
Helping Patients
In this field of medicine, continued refinements and change offer greater opportunity for infertile couples. Blastocyst culture is one important step and one at which FERTILITE excels. We have more than 20 years of experience in offering blastocyst transfers.